What is Spasticity?
Spasticity is a hardening of the muscles of the body. It is a common symptom in different types of neurological diseases, from cerebral palsy to multiple sclerosis, stroke or spinal cord injury and traumatic brain injury. Clinical treatment is often ineffective and invasive procedures may be required. It may be associated with spasms (as if the muscles jumped into a fright), and may be associated with pain.
What are the complications of Spasticity?
Spasticity can turn movements more difficult to be done, like walk, move a limb or do an activity. In severe cases, with constant and frequent contractions, the affected limbs may present shortening, assuming rigid positions, making daily activities difficult, making care, including personal hygiene, food, and other daily activities difficult. There may be pressure ulcers (skin sores, especially where supported), calcifications of the tendons, limiting the movement of the limbs, which appear hardened like stone, and stiffening of the joints. Urinary volume may be less and less, with urine leakage or even need for more frequent bladder catheterization. Pain is a complication of spasticity, as well as muscle atrophy, high energy expenditure. Cases of severe spasticity prevent the patient from assuming a position to use a wheelchair.
What is the treatment of spasticity?
The treatment of spasticity is carried out in a multidisciplinary team, with the participation of physiatrist, physiotherapist, occupational therapist, caregivers, family members, among others. When necessary intervention, initially the treatment is clinical, with the use of specific medications, and in the background, the patient can be submitted to interventional techniques, such as the application of toxin botulinum-A and neurolysis. The neurosurgeon has its role in the treatment of the most complex and refractory cases. Complications of spasticity may also require orthopedic treatment, plastic surgery, urologist, psychology, psychiatry, and social agents.
What are the major surgeries for treating spasticity?
The neurosurgeon performs some surgeries for the treatment of spasticity:
1) Baclofen pump implant (intrathecal)
2) Selective Dorsal Rhizotomy -SDR (treated in this section)
3) Other procedures are also performed for selected cases, like DREZotomy, intraventricular baclofen pump, intrathecal morphine pump, myelotomy among others.
You can read more about the procedures in this section: Surgeries for Treatment of Spasticity
What is Selective Dorsal Rhizotomy - SDR?
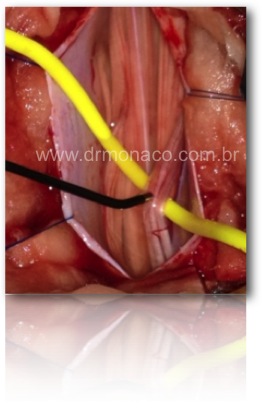
Selective dorsal rhizotomy - SDR, or superselective dorsal rhizotomy is a surgical procedure where the sensory afferents are diminished by surgical section of selected dorsal roots. This reduces the exacerbation of the medullary reflex arch, with consequent improvement in spasticity. Motor roots are preserved in this procedure, and also sensibility is preserved, because the sections are partials and the remaining rootlets provide all the information required for complete sensibility.
Dr. Bernardo de Monaco has been responsible for the spasticity outpatient clinic of the Hospital das Clínicas of the Faculty of Medicine of the University of São Paulo (Brazil) since 2012. This procedure arose in the early twentieth century, with constant technical improvements and has been performed by the functional neurosurgery team of the HCFMUSP since 1979, when Prof. Manoel Jacobsen Teixeira brought the technique of England. It can promote the improvement of spasticity (lower limbs or upper limbs) with functional improvement. This treatment is aimed at improving a symptom, called spasticity. It is not a treatment for a specific disease and it is not a cure.
This procedure continues to be performed in reference centers of spasticity treatment in the world, even with new techniques of neuromodulation, such as intrathecal or intraventricular baclofen infusion (baclofen pump).
It is important to consider that this procedure reduces spasticity. Many children use spasticity to be able to stand or even walk (when the weakness is severe). Spasticity is not always a symptom that have to be treated. A multidisciplinary evaluation is important to evaluate the real need for surgery and to evaluate other surgical possibilities. Patients candidates for SDR should have regular follow-up with a physiatrist, as well as be in rehabilitation preferably in a specialized clinic.
What are the main risks of Selective Dorsal Rhizotomy?
The main risks of this procedure are:
1) Cerebrospinal fluid leakage: As the surgery is performed inside the vertebral canal, within the dura mater, which is the membrane that surrounds the spinal cord, one of the possible complications of this surgery is the leakage of this liquid, called a CSF leakage. This leak can lead to difficult-to-treat headaches, and more severely, a contamination of the cerebrospinal fluid can happen with bacteria in the body, leading to postoperative meningitis. Contained fistulas (which do not leak through the skin) do not always need to be operated. Consult your surgeon about how to avoid CSF leak.
2) Pain: It is common to have pain in the region of the surgical wound after surgery. Intraoperative infiltration and blocks decrease this pain, which is usually more important in the first three days after surgery.
3) Numbness in the legs: for the procedure performed to treat spasticity in lower limbs, one of the complications is the sensation of numbness and tingling in the legs. It can last up to three months after the procedure. Few patients will experience discomfort associated with these numbness, called dysesthesia. Rarely is specific treatment required for this.
4) Loss of function of the sphincters: very rare. The selection of the radicles to be sectioned is of extreme importance. The section of the radicles of S2 to S4 are associated with loss of sexual function and loss of control of the sphincters, and the patient may present neurogenic bladder and intestine. Intraoperative electrophysiological monitoring is required and prevents such complications. In the technique adapted by Dr. Park, where only one level of the spine is opened for the procedure (technique modified and applied by Dr. Monaco), it is suggested to ever use neurophysiological monitoring.
5) Decreased leg strength: after SDR procedure it is possible that the improvement of spasticity occurs together with a decrease in strength in the affected limbs. The first explanation is that patient needs to re-learn how to use his strength without spasticity. Sometimes part of the force used by the patient is due to involuntary contractions associated with spasticity. It is important to alert the patient about this possibility before performing the procedure. Decreased strength is expected soon after the procedure, with improvement in days to weeks. Usually, the initial force is resumed after 6 months of the procedure, and may occur before or even two years after the procedure. After two years of surgery, there will be no further improvement.
6) Because the surgery is performed in horizontal ventral decubitus, with general anesthesia, there are operative risks inherent to all procedures involving this position, such as intraoperative bleeding, pain where the body is supported during surgery (in extreme cases, it may result in decubitus ulcer), and even (very rarely) postoperative blindness, never described for SDR, but described in spine surgeries. Unplanned complications can occur regardless of the surgical technique applied, it is always important to remember that medicine is not an exact science, so do not believe in a doctor who offers 100% certainty in any treatment.
7) In places where the intraoperative monitoring electrodes are placed, there are small holes, which may hurt or bleed soon after the procedure, without additional complications. Electrodes are used on various muscles of the body, which are usually tiny needles that pierce these muscles.
8) Spine deformity is a possible late complication, which consists of the development of a deformity in the spine where it spreads forward. This may occur most commonly using old surgery techniques where several levels of the spine were opened. With minimization to one level of opening, post-operative scoliosis has become more rare. Dr. Monaco currently, in addition to using only one level of access for surgery, performs the return of the posterior bone of the spine, technique called osteoplastic laminoplasty. The advantages of this technique are: less occurrence of cerebrospinal fluid leakage, less pain, less occurrence of deformities.
What are the main advantages of selective dorsal rhizotomy?
Of course, the most notable result is the improvement in spasticity in the lower limbs. This can be observed soon after the procedure, with sagging legs, much easier movement and without so much resistance. The force is usually diminished after the procedure, which is common and expected. The force may take up to 6 months to return, and in some cases may take up to two years. Intraoperative neurophysiological monitoring is essential and avoids cutting off motor roots, that is, those roots that bring strength to the lower limbs. Only the sensory roots selected are sectioned, which can lead to numbness or decreased sensitivity in the lower limbs, usually reversible after days or weeks. Sensibility stills the same after surgery, function is not just manteined, but it can be improved.
Secondarily, it can be observed: improvement of coordination and dystonia in the upper limbs, that is, children who had difficulties in using their hands, may present more easily; improvement in trunk balance; improvement of trunk spasticity; improvement in swallowing; improvement in spasms (sudden involuntary contractions); improvement in attention; less occurrence of deformities in limbs and less recurrency if operated; less need for medications for spasticity; less hospitalization due to the consequences of spasticity; less need for toxin botulinum type A; for patients with potential gait, there is gait facilitation, with the possibility of walking with support, or even without support, depending on two things: 1) baseline state of the patient before the procedure and 2) degree of improvement obtained after the procedure.
The following link contains pictures of surgeries and procedures that can impress the visitor. Caution is recommended!